Hysteroscopy for Infertility
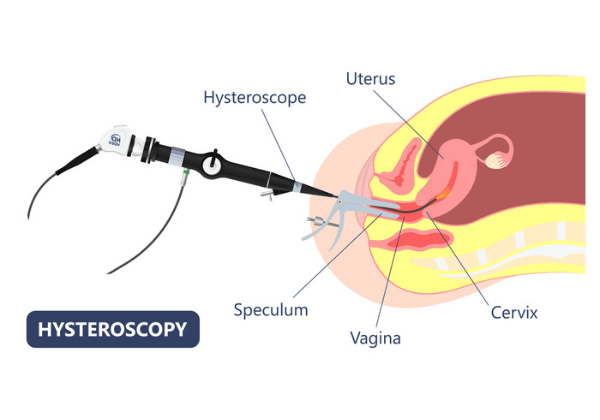
Hysteroscopy is used to identify and treat uterine disorders. A hysteroscopy is the most effective approach to determine whether your womb is healthy and capable of carrying a baby. A hysteroscopy is a long, thin, illuminated equipment introduced into the uterus through the vaginal canal. It also displays an image of the uterus on a screen, allowing the fertility doctor to examine it. Examination of the uterus cavity with hysteroscopy enables the identification and treatment of various uterine disorders. Some of which may cause fertility issues. In most cases, unsuccessful IVF attempts are due to problems in the embryo, such as genetic disorders or other difficulties with the woman’s uterus. Several fertility clinics have previously performed hysteroscopy on women who have had failed IVF cycles to look for uterine growths or scar tissues and remove them.
PSFC is proud to be at the forefront of what is to become the new standard for the minimally invasive removal of submucosal fibroids and endometrial polyps.
Leiomyomata or fibroids are the most common benign tumors of the uterus. They can cause a variety of symptoms, including painful periods, abnormally heavy (menorrhagia) or irregular (metrorrhagia) menses, pelvic pain, and infertility. Endometrial polyps are a common abnormality of the uterine lining. The uterine lining is made up of soft endometrial tissue that is shed each month if a woman does not become pregnant, causing menses, or a menstrual period. After a women’s period the lining rapidly grows back in order to support another possible pregnancy. Polyps are areas that grow too much, often resulting in a tree-like stalk with a larger bushy head attached to it. There can be single or multiple growths. These growths are diagnosed in approximately 20% of women with abnormal uterine bleeding. They can also interfere with proper implantation of the fertilized egg and may cause miscarriages if not removed.
Menorrhagia, heavy menstrual bleeding, is one of the most reported problems found by primary care physicians and gynecologists. It can severely impact a patient’s life by disrupting work, family and social events/time. If it is not treated it can lead to chronic anemia, pelvic pain, and cramping. Endometrial polyps and uterine fibroids are common causes of this abnormal bleeding, and if you are among those currently experiencing any of these symptoms you should get checked out by your doctor.
The old treatment for these growths ranged from the highly invasive hysterectomy for severe cases, to the often-ineffective dilation and curettage (D&C). Although these treatments are still widely used to treat menorrhagia, responsible for 20% of US hysterectomies and 40% of D&Cs, there are now other options. Recent advances have made hysteroscopic treatment a viable and more efficient option. Hysteroscopic myomectomy is now an effective method to remove small to moderate sized submucosal fibroids while hysteroscopic polypectomy is effective for endometrial polyps. In a conventional hysteroscopy the uterine cavity is first distended with non-electrolyte solution, then a resectoscope with a loop or ablating electrode is passed through the vagina into the uterus. The surgeon uses the resectoscope to remove any growths using an electro-surgical technique.
This type of hysteroscopy is less invasive than previous techniques, but it also has its disadvantages. The surgeon has to manually remove the cut tissue, which is time-consuming and potentially increases the risk of damaging the uterus. A big disadvantage is that the electrode loop often cannot remove the entire fibroid, which could mean repeating the procedure down the road. There is also the risk of thermal injury to surrounding tissue. Finally, the use of the non-electrolyte solution for distension of the uterus also raises the risk of sodium imbalances and fluid overloading.
The suction morcellator is the latest innovation that offers several key advantages over the resectoscope in the removal of fibroids and polyps. This new device takes away the need for the surgeon to constantly remove the cut tissue, as it can cut and remove tissue simultaneously. Taking away this time-consuming step throughout the procedure is a huge benefit to the patient as it results in a much-reduced operating time. A recent study showed that this new technique reduced average operating times for both the hysteroscopic removal of fibroids and polyps by half. This reduces the patient’s exposure to anesthesia, and greatly lowers the risk of fluid overloading. The risk of puncturing the uterus from multiple entries of surgical equipment is also reduced. More importantly, by using the suction morcellator our physicians can achieve complete removal of the fibroid or anomaly more often and with less damage to the uterus. This procedure allows the use of a saline solution to distend the uterus as the morcellator doesn’t make use of electric current to excise tissue; this reduces the risk of both electrolyte imbalance and thermal injury.
The use of the suction morcellator to perform operative hysteroscopy is, in our opinion, the new gold standard in the removal of submucosal fibroids and endometrial polyps. It decreases the risks of older techniques while offering a safer and more efficient removal of these growths. If you have been experiencing abnormal uterine bleeding, heavy painful periods, or have already been diagnosed with endometrial polyps or fibroids, call today to schedule a consultation with our highly trained staff.

