Egg is the quintessential part of a female reproductive system. You’re born with 1–2 million potential eggs (in the form of ovarian follicles). From this time, no new eggs are produced but that’s all the eggs you’ll ever have. Up to 1,000 eggs are lost each month. By puberty, your egg count might be half a million; at 25, maybe 300,000. Of these, only 300 to 400 will be ovulated during a woman’s reproductive lifetime. Fertility can drop as a woman ages due to decreasing number and quality of the remaining eggs. Then, around 35, the decline starts to get a bit steeper until all eggs have been depleted, a state known as Menopause. Most women reach menopause by the age of 50 but many healthy women reach menopause in their 40’s. Abnormally early menopause, or premature ovarian insufficiency, is when you run out of eggs before you should (before age 40).
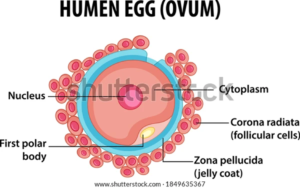
Cross-section of egg
Factors Affecting Egg Count:
Age, genetics, medical history, lifestyle
In addition to eggs being lost with age, they can be depleted or destroyed by certain medical treatments, such as chemotherapy or radiation for cancer, or by smoking, which can cause menopause to come up to 4 years earlier. Additionally, genetics comes into play—you’re 6 times more likely to experience early menopause if your mother, sister, or grandmother experienced it. There are also some rare genetic conditions, such as a Fragile X premutation or Turner mosaicism, that are associated with very early menopause.
Tests For Egg Count:
Measuring the levels of anti-Müllerian hormone, or AMH, in the blood. AMH is produced by the ovarian follicles, so the higher your AMH, the more follicles you have left. Additionally, a focused pelvic ultrasound for antral follicle count (AFC)—more visible follicles are typically indicative of a higher egg count.
Egg Quality
Egg quality refers to the genetic health of an egg. The eggs inside your ovaries are “primordial,” or immature eggs. Before you ovulate, they go through another phase of cell division, called meiosis. During this phase, an individual egg can either divide correctly and become healthy (genetically normal, also known as euploid) or divide incorrectly and become unhealthy (genetically abnormal, also known as aneuploid).
Since genetic material—DNA—is like an instruction manual for our cells, any errors in a cell’s DNA can prevent it from doing what it’s supposed to do. Abnormal egg cells typically don’t fertilize or implant in the uterus, but in the rare case they do, they can result in miscarriage or genetic disorders like Down syndrome.
Factors Affecting Egg Quality:
Age, medical history (maybe)
Older eggs are more likely to accumulate errors in their DNA during meiosis, leading to genetically abnormal eggs. That means, as you age, a higher and higher percentage of the eggs inside your ovaries will contain genetic abnormalities. This is why we see infertility, miscarriage, and genetic disorders much more often with women over 35.
It’s theorized that some reproductive illnesses, such as endometriosis, may also affect egg quality—but the relationship isn’t totally clear just yet.
Tests For Egg Quality:
There’s no test for egg quality, but because egg quality declines naturally and inevitably with age, your age is a good proxy for the percentage of normal eggs you have. Fertilized eggs (embryos) can be genetically tested using a procedure called preimplantation genetic screening/diagnosis (PGS or PGD).