Female Infertility Treatment
Female infertility accounts for more than 40% of the infertility problems observed in couples. Symptoms, diagnosis of the causes and treatment thereof have been well developed. To understand infertility issues in women, it is important to understand Female reproductive system and the elements thereof.
Female Reproductive System
The female reproductive system provides several functions. The ovaries produce the egg cells, called the ova or oocytes. The oocytes are then transported to the fallopian tube where fertilization by a sperm may occur. The fertilized egg then moves to the uterus, where the uterine lining has thickened in response to the normal hormones of the reproductive cycle. Once in the uterus, the fertilized egg can implant into thickened uterine lining and continue to develop. If implantation does not take place, the uterine lining is shed as menstrual flow. In addition, the female reproductive system produces female sex hormones that maintain the reproductive cycle.
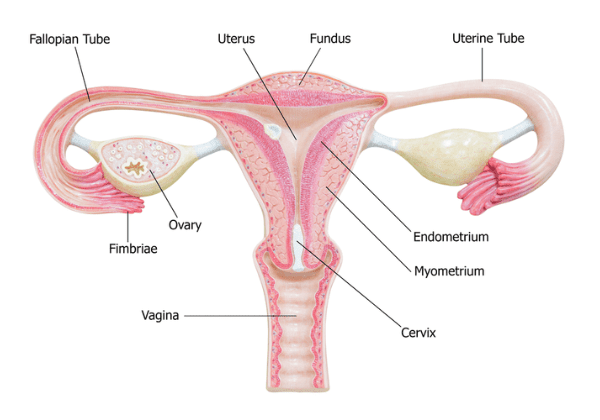
The internal reproductive organs include:
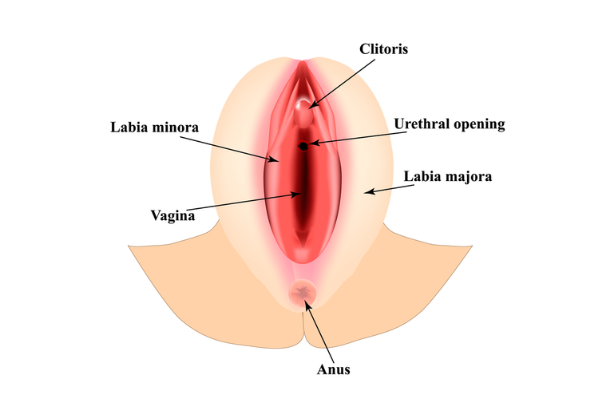
- Vagina: The vagina is a canal that joins the cervix (the lower part of uterus) to the outside of the body. It also is known as the birth canal.
- Uterus (womb): The uterus is a hollow, pear-shaped organ that is the home to a developing fetus. The uterus is divided into two parts: the cervix, which is the lower part that opens into the vagina, and the main body of the uterus, called the corpus. The corpus can easily expand to hold a developing baby. A canal through the cervix allows sperm to enter and menstrual blood to exit.
- Ovaries: The ovaries are small, oval-shaped glands that are located on either side of the uterus. The ovaries produce eggs and hormones.
- Fallopian tubes: These are narrow tubes that are attached to the upper part of the uterus and serve as pathways for the ova (egg cells) to travel from the ovaries to the uterus. Fertilization of an egg by a sperm normally occurs in the fallopian tubes. The fertilized egg then moves to the uterus, where it implants to the uterine lining.
What happens during the menstrual cycle?
Females of reproductive age (beginning anywhere from 11 to 16 years of age) experience cycles of hormonal activity that repeat at about one-month intervals. Menstru means "monthly” – leading to the term menstrual cycle. With every cycle, a woman’s body prepares for a potential pregnancy, whether or not that is the woman’s intention. The term menstruation refers to the periodic shedding of the uterine lining. Many women call the days that they notice vaginal bleeding their “period,” “menstrual” or cycle.
The average menstrual cycle takes about 28 days and occurs in phases. These phases include:
- The follicular phase (development of the egg)
- The ovulatory phase (release of the egg)
- The luteal phase (hormone levels decrease if the egg does not implant)
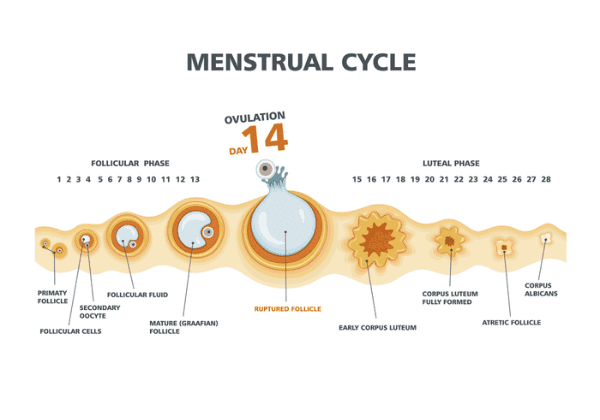
Follicular phase
This phase starts on the first day of your period. During the follicular phase of the menstrual cycle, the following events occur:
- Two hormones, follicle stimulating hormone (FSH) and luteinizing hormone (LH) are released from the brain and travel in the blood to the ovaries.
- The hormones stimulate the growth of about 15 to 20 eggs in the ovaries, each in its own “shell,” called a follicle.
- These hormones (FSH and LH) also trigger an increase in the production of the female hormone estrogen.
- As estrogen levels rise, like a switch, it turns off the production of follicle-stimulating hormone. This careful balance of hormones allows the body to limit the number of follicles that will prepare eggs to be released.
- As the follicular phase progresses, one follicle in one ovary becomes dominant and continues to mature. This dominant follicle suppresses all of the other follicles in the group. As a result, they stop growing and die. The dominant follicle continues to produce estrogen.
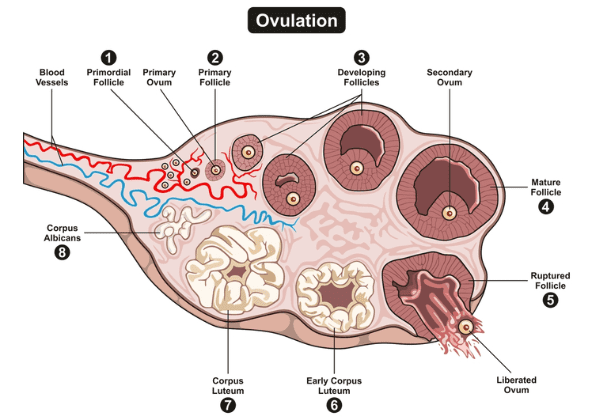
Ovulatory phase
The ovulatory phase (ovulation) usually starts about 14 days after the follicular phase started, but this can vary. The ovulatory phase falls between the follicular phase and luteal phase. Most women will have a menstrual period 10 to 16 days after ovulation. During this phase, the following events occur:
- The rise in estrogen from the dominant follicle triggers a surge in the amount of luteinizing hormone that is produced by the brain.
- This causes the dominant follicle to release its egg from the ovary.
- As the egg is released (a process called ovulation) it is captured by finger-like projections on the end of the fallopian tubes (fimbriae). The fimbriae sweep the egg into the tube.
- For one to five days prior to ovulation, many women will notice an increase in egg white cervical mucus. This mucus is the vaginal discharge that helps to capture and nourish sperm on its way to meet the egg for fertilization.
Luteal phase
The luteal phase begins right after ovulation and involves the following processes:
- Once it releases its egg, the empty ovarian follicle develops into a new structure called the corpus luteum.
- The corpus luteum secretes the hormones estrogen and progesterone. Progesterone prepares the uterus for a fertilized egg to implant.
- If intercourse has taken place and a man’s sperm has fertilized the egg (a process called conception), the fertilized egg (embryo) will travel through the fallopian tube to implant in the uterus. The woman is now considered pregnant.
- If the egg is not fertilized, it passes through the uterus. Not needed to support a pregnancy, the lining of the uterus breaks down and sheds, and the next menstrual period begins.
Factors Affecting Ovulation:
Age, hormonal imbalances, lifestyle factors
Because you have fewer eggs as you age, ovulation can become less regular, especially in perimenopause (the 5–10 years leading up to menopause).
Ovulation can also be impacted by an imbalance in the hormones that control the process, such as in polycystic ovary syndrome, or by obesity, malnutrition, sleep disruption, stress, or other lifestyle factors that alter hormone levels.
Test For Ovulation:
Ovulation predictor kits, blood tests, and ultrasounds.
Possible Treatments:
Medication to induce ovulation

Symptoms To Female Infertility:
The main symptom of infertility is the inability to get pregnant within 12 months of regular unprotected sex. A menstrual cycle that’s too long (35 days or more), too short (less than 21 days), irregular or absent can mean that you’re not ovulating. Recurrent Pregnancy Failure (Two or more pregnancy losses in a row) could also be a symptom to infertility.
For pregnancy to occur, every step of the human reproduction process must happen correctly. The steps in this process are:
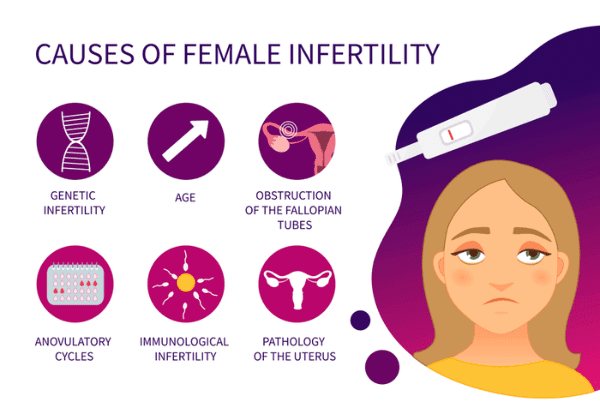
Ovulation disorders
Ovulating infrequently or not at all (anovulation) accounts for most cases of infertility. Problems with the regulation of reproductive hormones by the hypothalamus or the pituitary gland or problems in the ovary can cause ovulation disorders.
- Polycystic ovary syndrome (PCOS).PCOS causes a hormone imbalance, which affects ovulation. PCOS is associated with insulin resistance and obesity, abnormal hair growth on the face or body, and acne. It’s the most common cause of female infertility.
- Hypothalamic dysfunction.Two hormones produced by the pituitary gland are responsible for stimulating ovulation each month — follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Excess physical or emotional stress, a very high or very low body weight, or a recent substantial weight gain or loss can disrupt production of these hormones and affect ovulation. Irregular or absent periods are the most common signs.
- Primary ovarian insufficiency.Also called premature ovarian failure, this is usually caused by an autoimmune response or by premature loss of eggs from your ovary, possibly as a result of genetics or chemotherapy. The ovary no longer produces eggs, and it lowers estrogen production in women under age 40.
- Too much prolactin.The pituitary gland can cause excess production of prolactin (hyperprolactinemia), which reduces estrogen production and can cause infertility. This can also be caused by medications you’re taking for another condition.
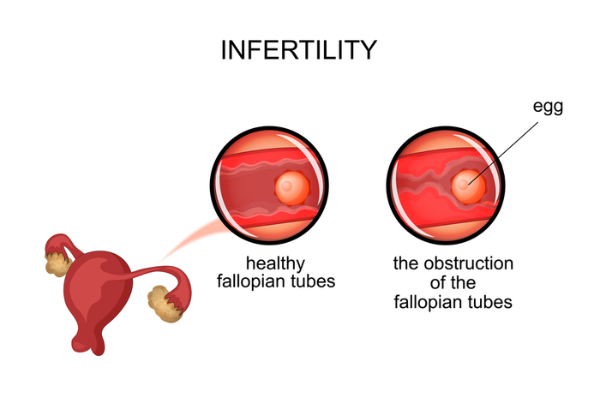
Damage to fallopian tubes (tubal infertility)
Damaged or blocked fallopian tubes keep sperm from getting to the egg or block the passage of the fertilized egg into the uterus. Causes of fallopian tube damage or blockage can include:
- Pelvic inflammatory disease, an infection of the uterus and fallopian tubes due to chlamydia, gonorrhea or other sexually transmitted infections
- Previous surgery in the abdomen or pelvis, including surgery for ectopic pregnancy, in which a fertilized egg implants and develops somewhere other than the uterus, usually in a fallopian tube
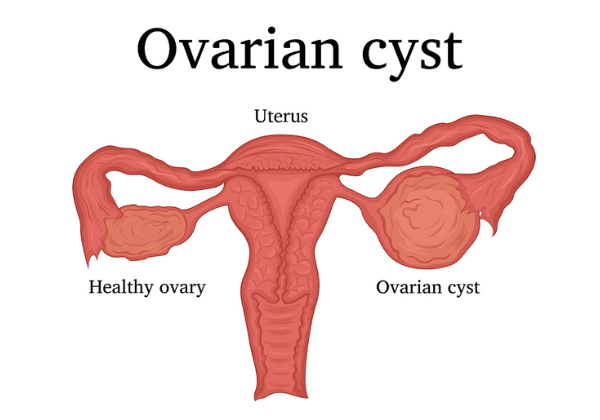
Ovarian cysts
Ovarian cysts that can affect your fertility include:
- Endometriomas. Endometriomas are cysts caused by endometriosis, a condition in which the tissue normally lining your uterus (endometrium) grows outside the uterus. This extra tissue growth — and the surgical removal of it — can cause scarring, which can block fallopian tubes and keep an egg and sperm from uniting. Endometriosis can also disrupt implantation of the fertilized egg. The condition also seems to affect fertility in less-direct ways, such as damage to the sperm or egg.
- Ovarian cysts resulting from polycystic ovary syndrome.Polycystic ovary syndrome (PCOS) is a condition marked by many small cysts on your ovaries, irregular periods and high levels of certain hormones. PCOS is associated with irregular ovulation, which may contribute to problems with fertility in some women.
Uterine or cervical causes
Several uterine or cervical causes can interfere with the egg implanting or increase the risk of miscarriage:
- Benign polyps or tumors (fibroids or myomas) are common in the uterus. Some can block fallopian tubes or interfere with implantation, affecting fertility. However, many women who have fibroids or polyps do become pregnant.
- Problems with the uterus present from birth, such as an unusually shaped uterus, can cause problems becoming or remaining pregnant.
- Cervical stenosis, a narrowing of the cervix, can be caused by an inherited malformation or damage to the cervix.
- Sometimes the cervix can’t produce the best type of mucus to allow the sperm to travel through the cervix into the uterus.
Unexplained infertility
In some cases, the cause of infertility is never found. A combination of several minor factors in both partners could cause unexplained fertility problems. Although it's frustrating to get no specific answer, this problem can correct itself with time. But you shouldn't delay treatment for infertility.
Diagnostic tests:
- TEST FOR HARMONE LEVELS:
Anti-Mullerian Hormone (AMH) test through blood sample.
This hormone is secreted by the pre-antral and small antral follicles in the female ovary. These are small follicles that can later grow into mature follicles which produce the oocytes (eggs) that will be required for your pregnancy. AMH is only produced by these very small follicles that are not detectable by ultrasound or other hormone markers such as FSH and Inhibin B. These levels are very low in women who have diminished ovarian reserve and very high in women who may have polycystic ovarian syndrome (PCOS). As such, it is a useful marker to help us determine the quantity and quality of the follicles remaining in the ovary. This is referred to as your ovarian “reserve.”
We have found this test to be tremendously useful. We use the results in combination with several other markers and procedures to determine the most appropriate course of therapy. AMH will provide an additional piece of very useful and specific information about your available egg supply, essentially functioning as an early warning system alerting to the possibility of decreased fertility potential.
- TESTS FOR FALLOPIAN TUBE HEALTH:
An HSG (hysterosalpingogram) is normally conducted to assess the quality of Fallopian tube
- TESTS FOR UTERINE HEALTH:
Regular ultrasound or saline infusion sonogram can identify abnormalities of the uterus, growths within the uterus, and the thickness of the uterine lining. Endometrial biopsy can evaluate the uterine lining for abnormal cells and proper hormone levels.
Treatments for Female Infertility
Treatment options will depend on the cause of the initial problem, age of the woman, history of any previous pregnancies, the male factor, and how long infertility issues have been known. Below are some common treatment options when it comes to female infertility
Hormone Medications:
-
- Medications for ovarian stimulation. To stimulate your ovaries, you might receive an injectable medication containing a follicle-stimulating hormone (FSH), a luteinizing hormone (LH) or a combination of both. These medications stimulate more than one egg to develop at a time.Oral medication that allows the female body to produce more of the hormones (AMH) that cause the eggs to mature in their ovaries.
- Medications for oocyte maturation. When the follicles are ready for egg retrieval — generally after eight to 14 days — you will take human chorionic gonadotropin (HCG) or other medications to help the eggs mature.
- Medications to prevent premature ovulation. These medications prevent your body from releasing the developing eggs too soon.
- Medication for triggering the release of egg from the follicle ‘trigger shot’ that allows for the final maturation of the follicles and readies the eggs for release
- Medications to prepare the lining of your uterus. On the day of egg retrieval or at the time of embryo transfer, your doctor might recommend that you begin taking progesterone supplements to make the lining of your uterus more receptive to implantation
Surgical Treatments:
May become unavoidable when it comes to the following infertility causes:
- Disease of the fallopian tubes: Surgery can repair or remove blockages.
- Ectopic pregnancy, which is when the pregnancy occurs outside of the uterus: Surgery of the fallopian tube is done in an effort to help fix these tubal pregnancies.
- Patches of endometriosis: Surgery is done to help remove these patches, doubling the chances of a pregnancy. Surgery can also be done in an effort to remove scarring, polyps, or uterine fibroids.
Risk factors
Certain factors may put you at higher risk of infertility, including:
- The quality and quantity of a woman’s eggs begin to decline with age. In the mid-30s, the rate of follicle loss speeds, resulting in fewer and poorer quality eggs. This makes conception more difficult and increases the risk of miscarriage.
- Besides damaging your cervix and fallopian tubes, smoking increases your risk of miscarriage and ectopic pregnancy. It’s also thought to age your ovaries and deplete your eggs prematurely. Stop smoking before beginning fertility treatment.
- Being overweight or significantly underweight may affect ovulation. Getting to a healthy body mass index (BMI) might increase the frequency of ovulation and likelihood of pregnancy.
- Sexual history.Sexually transmitted infections such as chlamydia and gonorrhea can damage the fallopian tubes. Having unprotected sex with multiple partners increases your risk of a sexually transmitted infection that may cause fertility problems later.
- Excess alcohol consumption can reduce fertility.
Prevention
For women thinking about getting pregnant soon or in the future, these tips might help:
- Maintain a healthy weight.Overweight and underweight women are at increased risk of ovulation disorders. If you need to lose weight, exercise moderately. Strenuous, intense exercise of more than five hours a week has been associated with decreased ovulation.
- Quit smoking.Tobacco has multiple negative effects on fertility, as well as your general health and the health of a fetus. If you smoke and are considering pregnancy, quit now.
- Avoid alcohol.Heavy alcohol use may lead to decreased fertility. And any alcohol use can affect the health of a developing fetus. If you’re planning to become pregnant, avoid alcohol, and don’t drink alcohol while pregnant.
- Reduce stress.Some studies have shown that stress can cause couples to have poorer results with infertility treatment. Try to reduce stress in your life before trying to become pregnant.

